2019 legislative session
Governor signs into law legislation to prevent another behavioral health scandal
|
Gov. Michelle Lujan Grisham signed into law this week a bill (SB41) that ensures service providers accused of overbilling or defrauding Medicaid can review and respond to allegations of wrongdoing before state action is taken.
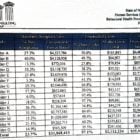
It’s a response to the bombshell announcement the administration of Gov. Susana Martinez made in June 2013. That summer, the Human Services Department publicly accused 15 organizations treating New Mexicans for addiction and mental illness of overbilling Medicaid by up to $36 million. There was even a chance, the agency said, the organizations had defrauded the government’s health insurance program for low-income people. The organizations weren’t allowed to review or respond to audit findings that led to the allegations – a break with normal auditing practices – or dispute the state Human Services Department’s decision to cut off Medicaid funding to a dozen or so of the 15 providers.